Document Type : Review Article
Authors
- Solmaz Maleki Dizaj 1, 2
- Simin Sharifi 2
- Shahriar Shahi 2, 3
- Soheila Montazersaheb 4
- Sara Salatin 2
- Elham Ahmadian 5
- Khadijeh Khezri 6
- Yalda Rahbar Saadat 5
- Elaheh Dalir Abdolahinia 7
- Mohammad Ali Ghavimi 8
1 Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran
2 Dental and Periodontal Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
3 Department of Endodontics, Faculty of Dentistry, Tabriz University of Medical Sciences, Tabriz, Iran
4 Molecular Medicine Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
5 Kidney Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
6 Deputy of Food and Drug Administration, Urmia University of Medical Sciences, Urmia, Iran
7 Research Center for Pharmaceutical Nanotechnology, Biomedicine Institute, Tabriz University of Medical Sciences, Tabriz, Iran
8 Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Tabriz University of Medical Sciences, Tabriz, Iran
Abstract
The main goal of this study was to gather the most critical bioactivities of curcumin, followed by the most essential concerns in its clinical usage and the challenges and potential for its use in modern medical studies. The conducted clinical studies on curcumin showed an effective anti-inflammatory and anti-cancer agent. The search results also revealed that curcumin has poor systemic bioavailability. Then, designing new methods to improve its bioavailability has always been interesting. Other conditions, such as neurodegenerative disease, cardiovascular disease, and diabetes, should be the subject of additional clinical research in the future. Besides, new procedures, such as adjuvants, drug delivery systems, and structural changes should be used in clinical trials of curcumin.
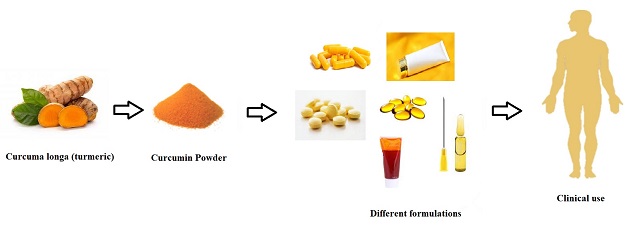
Graphical Abstract
Keywords
Main Subjects
Introduction
Medicinal plants have shown a critical part in the progress of human culture [1]. They have always been popular because of their lack of toxicity. Medicines derived from these items serve a significant role in human healthcare and preventing illnesses [2]. Natural products are claimed to be used by 80 percent of developing countries to improve their overall health [3]. Abundant herbal active ingredients such as flavonoids, phytoalexins, and phenolic compounds have been applied as adjuvants in treating diseases, for example, cancer chemotherapy [4,5]. Fewer side effects are essential benefits of applying natural phytochemicals and polyphenols [6].
Curcumin is a key component of Curcuma longa (also called turmeric). It has been applied in Eurasian countries to treat many diseases [7]. The European explorers brought it to Western culture in the 14th century [8]. Curcumin occurs in equilibrium with its enol tautomer. Composition of commercial turmeric: 77% diferuloylmethane (curcumin), 17% demethoxycurcumin, and 3% bisdemethoxycurcumin [9]. For centuries, people have been using turmeric as a traditional medicine to heal different skin conditions, cure dental infections, digestive complaints, and numerous wounds [10]. Curcumin can also be used as an authorized food additive to improve the color and flavor of food [7-9]. It was only newly that researchers began looking at how curcumin works to cure various illnesses [11,12]. Scientists have discovered curcumin's wide variety of bioactivities, and its ability to fight oxidative stress and inflammation as well as cancer and microbial infections [13-15].
Clinical studies include investigations based on dosage, timing, and other essential factors. An overview of online databases displays that the therapeutic properties of curcumin have been thoroughly investigated in several clinical trials. So, curcumin can be preferred over other medicinal plants for therapy of some diseases such as cancer on human participants to progress medical knowledge [16].
In the first step, a clinical study should be planned ethically and methodically to keep the participants' health [17, 18]. Clinical trials in humans are designed to guarantee the effectiveness and safety of a new intervention (in a new drug or medical device) [19].
During this review, the most critical bioactivities of curcumin will be reviewed, followed by the most important concerns in its clinical usage and the challenges and potential for its use in modern medical studies
Curcumin chemistry
Chemical structure
The Curcuma longa plant produces curcumin, a brilliant yellow compound. Turmeric (Curcuma longa or Turmeric), a Zingiberaceae ginger family member, contains the principal curcuminoid curcumin. It is available as a herbal supplement, cosmetic ingredient, food flavoring, and food coloring [20,21]. Turmeric's yellow hue is due to curcumin, a diarylheptanoid that belongs to the curcuminoids family of phenolic pigments [22]. Figure 1 reveals the chemical structure of curcumin.
Extraction of curcuminoids from Turmeric
Curcumin may be extracted from turmeric in various methods, according to research in the literature [23]. Because curcuminoids are not water-soluble, extractions must be done in nonpolar solvents. Hexane, acetone, ethylene dichloride, and other alcohols have previously been used to extract curcumin mimics. Acetone extraction has been demonstrated to provide the most remarkable outcomes [23]. A soxhlet device is one technique for extracting chemicals, which implies that the extraction and filtering of the result are done in the same step. Turmeric powder is placed in a paper thimble in a glass container. When the heated solvent vapor reaches the glass container, it condenses and fills it. The filtrate will flow back to the round bottom flask holding the solvent when the volume of the extract surpasses a predetermined threshold. The extraction is complete when the filtrate is colourless [24]. Another method is to dissolve the turmeric powder in acetone and mix it for many hours to extract the curcuminoids. The solution is filtered to remove any unresolved material from the turmeric powder. High performance liquid chromatography (HPLC) with an appropriate mobile phase may be used to determine the number of curcuminoids. However, column chromatography with a suitable mobile phase is required to separate the compounds in higher proportions. After a series of investigations on Thin-layer chromatography (TLC) with Ultraviolet (UV) detection, the mobile phase is selected to get the optimum Rf values for curcuminoid separation. Curcuminoids that have previously been refined and separated may be purified via crystallization [25].
Synthesis of curcumin
Curcumin may also be produced by synthesizing it. Vanillin, acetylacetone, and boron oxide are common ingredients. In the first stage, acetylacetone reacts with boron oxide to generate the boron complex [15]. The complex's goal is to make the methylene group between the carbonyls less nucleofilic, lowering its reactivity. The terminal methyl groups will participate in the following aldol reaction instead of the methylene due to the shielding [6,16]. In a typical aldol condensation, using n-butyl amine to remove a hydrogen atom from one of the methyl groups causes the carbon to serve as a nucleophile on the carbonyl carbon in the vanillin. Due to the ease with which the molecule may form the conjugated system, the resultant aldol product will most likely be dehydrated through an E1cB mechanism. In the last stage, a hydrochloric solution will eliminate the boron complex. Another way to make curcumin is to use a microwave oven to perform a microwave-assisted reaction using the same ingredients. [14] Heat goes through the vessel wall before reaching the content in traditional heating. This method takes time and effort. The dipoles of the molecules spin to align with the electric field created by the microwaves churning the contents. Because the responsive chemical interacts directly, the temperature will increase instantly due to this activity. The heating is more constant, and the heating time is shorter. It is also faster and more environmentally friendly than traditional heating since it requires little or no solvent. In microwave-assisted procedures, the anticipated product yields are several times greater [16,17]. However, these processes can overheat, and determining the best moment to stop irradiation may be difficult.
Curcumin bioactivities
Antimicrobial Action
Some surveys have shown curcumin antiviral, antifungal, antibacterial, and antimalarial actions. Because of the wide-ranging antimicrobial activities of this beneficial herbal agent, it was applied as a basis for the production of antimicrobial agents [26,27]. Previous investigations also displayed that the local applications of curcumin gel reduced inflammation and decreased the disease severity [28-32]. Curcumin was shown in many animal studies to have antibacterial [31,33], antifungal [34,35], antiviral [36], and activities. In Swiss mice, oral curcumin caused a 90% decrease in parasitemia and a 29% increase in overall survival Berghei [37]. Curcumin's impact may be a consequence of its capacity to encourage cell apoptosis and decrease cell proliferation [38].
Several reports show that curcumin inhibited bacteria by damaging bacterial membrane [39-41]. Curcumin has also been revealed to inhibit bacterial cell proliferation by perturbating FtsZ assembly. Other studies also demonstrate that curcumin can profoundly deactivate bacteria by encouraging ROS bacteria production by encouraging ROS production, including singlet oxygen and hydroxyl radicals [42,43].
Antioxidant property
Oxidative damage and oxidative stress contribute to several pathological conditions, including atherosclerosis [44-46] and myocardial ischemia [47,48]. One of the critical factors involved in cellular damage of those pathological conditions is reactive oxygen species (ROS) [49,50]. Administration of curcumin leads to direct removal of ROS in red cells and peritoneal macrophages of rats [51]. Curcumin elevates the expression and action of heme oxygenase-1 (HO-1) [52-54], which can degrade heme and produce the antioxidant biliverdin. Nevertheless, high doses and chemical environment may cause curcumin to act as a pro-oxidant. Thus, the balance between the antioxidant and pro-oxidant seems crucial in curcumin applications [55,56].
Cell apoptosis induction
The reports demonstrate that curcumin can induce apoptosis, particularly in cancerous cells through DNA damage [57,58], which provokes cytochrome c release and subsequent caspase activation [58-60]. Several cell survival signaling pathways mediated by NF-κB, Akt, and numerous cell survivals-associated proteins are implicated in these procedures. Curcumin may inhibit NF-κB activation probably through various steps including quenching reactive oxygen intermediates (ROI), suppression of the expression and action of downstream cyclooxygenase-2 (COX-2), the X-linked inhibitor of apoptosis protein Bcl-XL and anti-apoptotic proteins Bcl-2, and several cytokines [61, 62]. Furthermore, curcumin inhibits the Akt pathway by damaging its phosphorylation [58, 63]. Following curcumin treatment in human basal cell carcinoma, overexpression of P53 and subsequent cell apoptosis happens [64]. Additionally, curcumin leads to DNA damage-inducible (GADD) genes upregulation as well as survival genes (i. e. egr-1, cmyc, IAP (inhibitor of apoptosis protein), and their related proteins) downregulation. Besides, curcumin induces apoptosis through bcl-2 down-regulation and increased mitochondrial membrane permeability [65,66],
Anti-cell adhesion and anti-angiogenesis
Cell adhesion is an important phenomenon in various physiological and pathological events, and it is known as a prerequisite step for the invasion of cancer cells. The specific interactions mediate this complex process between receptors and extracellular glycoproteins. The best-established cell adhesion receptors are integrins. According to a literature review, curcumin applies its pharmacological actions through a wide diversity of mechanisms. Curcumin can suppress crosstalk between signaling molecules and adhesion molecules such as integrins. Some reports have revealed that curcumin treatment negatively affects the expression levels of two crucial cell adhesion molecules, β-catenin, and E-Cadherin. Curcumin inhibits cell migration by amplifying a negative feedback loop of E-cadherin and beta-catenin [67, 68]. There are also several studies indicating that curcumin could reduce the expression level of adhesion molecules like intercellular adhesion molecule-1 (ICAM-1, CD54) [69], vascular cell adhesion molecule-1 (VCAM-1, CD106) [70], and E-selectin (CD62), in that way cellular adhesiveness to the extracellular matrix is decreased [71].
It is believed that these surface adhesion molecules can regulate vascular endothelial cells, the production and release of pro/anti-inflammatory factors, and the migration of inflammatory cells to various tissues and organs. In support of this view, some studies claim curcumin can inhibit the transmembrane receptor α6β4 integrin, which is known to be essential for the motility and invasion of breast cancer. α6β4 was initially described as a receptor for the laminin family members. Additionally, curcumin can inhibit nuclear factor-kB and Akt, which are downstream effectors of α6β4 [72].
Another study found that curcumin inhibited lung cancer cells' invasion and metastatic spread. Indeed, curcumin effects are mediated by activation of HLJ1, as a novel member of DnaJ-like heat shock protein 40 (HSP40). HLJ1is a tumor suppressor that inhibits cell proliferation, invasion, and motility in lung cancer cells, and its overexpression is strongly linked to a reduced risk of lung cancer recurrence. Curcumin treatments result in up-regulation of HLJ via activation of the JNK/JunD pathway and modulation of E-cadherin expression, indicating anti-invasive and antimetastatic effects of curcumin [73].
Visfatin is an adipokine secreted mainly by adipose tissues and plays a pivotal role in the development and progression of breast cancer. The nuclear factor (NF)-κB signaling pathway is a significant target for curcumin. Relying on this fact, NF-κB directly regulates the gene expression of visfatin, as a downstream target of NF-κB signaling. Based on in vitro analysis, curcumin could decrease the activity of NF-κB and reduce the level of vistafin, implicating the protective role of curcumin against breast cancer invasiveness [74].
Interestingly, some studies have reported that curcumin treatment results in significant alterations in cell motility in some cancer cell lines. Relying on this fact, curcumin exhibited profound effects on actin-based motility and microfilament organization in both PC-3 and LNCaP prostate cancer cell lines. Aside from this, curcumin protected f-actin against disruption by cytochalasin B. Collectively, curcumin could antagonize the effects of neoplastic agents involved in perturbing actin dynamics [75].
Converging evidence has shown that angiogenesis has a fundamental role in developing tumor growth and tumor-associated metastasis. Without angiogenesis, a primary tumor can grow only 1–2 mm3 [76]. It is well documented that hypoxia is a crucial mediator of angiogenesis. Under hypoxic conditions, hypoxia-inducible factor 1 (HIF-1) is produced or activated. HIF-1 activation stimulates angiogenesis, thereby HIF-1 can be used as the target in cancer therapy [77].
In vitro and in vivo research on curcumin has revealed anti-oxidant activity. There is emerging evidence that curcumin could dramatically decrease hypoxia-induced angiogenesis through down-regulation of HIF-1 in a model of hepatocellular carcinoma. This leads to a reduction in the level of vascular endothelial growth factor (VEGF), as a main angiogenic factor [78].
In addition to VEGF, cancer cells overexpress pro-angiogenic factors, such as epidermal growth factor (EGF), fibroblast growth factor (FGF), angiopoietins (Ang) which contribute to the formation of blood vessels [79].
Furthermore, matrix metalloproteinases (MMPs) play a crucial role in angiogenesis and tumor metastasis via degrading and remodeling of the extracellular matrix. These events facilitate the invasion and metastatic behavior of cancer cells. Along with this view, it was revealed that curcumin could down-regulate matrix-degrading enzymes through inhibition of NF-κB activity and transcriptional downregulation of AP-1. Overall, the reduced NFκB/AP-1 activity and MMP level could diminish lung metastasis in a mice model of breast cancer [80].
The anti-angiogenic effect of curcumin was also observed in the Ehrlich ascites carcinoma tumor model. Following curcumin treatment, the level of VEGF was significantly decreased. Furthermore, the combination of curcumin with carboplatin exerts an anti-angiogenic effect by inhibiting VEGF and VEGF receptor Type 2, suggesting curcumin may be beneficial in cancer treatment through inhibition of angiogenesis [81].
Clinical bioavailability of curcumin
In a clinical trial, Cheng et al. examined the concentration of curcumin in serum of twenty-five patients with high-risk pre-malignant lesions by high-pressure liquid chromatography (HPLC). They reported that the maximum serum concentration of curcumin was recorded at one to two hours after oral consumption. These authors revealed that the use of 4 g, 6 g, and 8 g of oral curcumin produced a peak serum concentration of 0.51±0.11 μM, 0.63±0.06 μM, and 1.77±1.87 μM, respectively. However, its concentration decreased moderately during 12 hours. This study demonstrated that at doses below 4 g of curcumin, the peak of curcumin in the serum could not be detected, and it was also not found in urine [82]. In line with these results, the authors highlight poor intestinal absorption of curcumin.
In another clinical trial study, oral curcumin (3.6 g daily) was administrated on 6 patients with colorectal cancer. The consequences revealed that the plasma concentration of curcumin was detectable in only three patients with a mean of 11.1±0.6 nM. High levels of curcumin and its metabolites in the urine were observed for the 3.6 g dose group (daily) of oral curcumin. Pharmacokinetics parameters were constant in volunteers during the first month of oral consumption of curcumin. Outcomes of oral delivery studies of 3.6 g curcumin daily in patients showed that curcumin and its metabolites could be detectable through ADME (absorption, distribution, metabolism, and excretion in the urine) properties [83,84].
In one patient's liver tissue, trace amounts of hexahydrocurcuminol and hexahydrocurcumin, curcumin's metabolic product, were detected, but curcumin was not detected [84]. Another research conducted by the same group discovered that curcumin concentrations in normal and cancerous colorectal tissue were 12.7±5.7 and 7.7±1.8 nM/g, respectively, once patients received 3600 mg curcumin [85]. Apart from the studies on patients with different illnesses, researchers examined the pharmacokinetics of curcumin conjugate metabolites in healthy human volunteers [86]. Six subjects received 10 g of curcumin, while the remaining six received 12 g. At 14 time points, the amount of curcumin and its glucuronide and sulfate conjugates in serum was determined. Free curcumin was found in the plasma of one individual 30 minutes after 10 g of the medication was administered. On the other hand, curcumin conjugates were detected in the serum of all individuals [86].
Then, oral curcumin treatment at dosages up to 3600 mg may result in detectable curcumin and its metabolites in plasma and urine. Curcumin was absorbed and metabolized in a specific quantity. Optimal medicinal properties require an oral dose of more than 8 grams per day [87,88]. However, preclinical models and clinical investigations on volunteers and patients have shown that oral treatment leads to poor systemic bioavailability. As a result, specific techniques for increasing its absorption and overcoming its low bioavailability are required, described later.
Clinical safety of curcumin
Numerous clinical trials have been conducted to evaluate curcumin, as broad positive effects have been found in both in vitro and in vivo conditions. Translating preclinical effects to the clinic is critical to further confirm the feasibility and efficacy of such products in clinical applications [89]. The evaluation of the safety of curcumin in the context of clinical trials was initially reported in 2001 in a study, which involved 25 arsenic Bowen’s disease, bladder cancer resected, stomach metaplasia, uterine cervical intraepithelial neoplasm, and oral leukoplakia patients [90]. In this study, different doses of curcumin (500, 1000, 2000, 4000, and 8000 mg/day) were prescribed orally for three months. Administration of higher concentrations of curcumin was not possible due to the formation of the bulky volume of the formulated tablets.
Additionally, no toxic effect was observed in using curcumin at the highest concentration in this study [90]. Two other studies have assessed the safety of curcumin in colorectal cancer patients. The first study included a dose-escalation pilot trial in advanced colorectal cancer patients (n=15) in which capsules containing 400-2200 mg curcuma extracts were administrated. These capsules encompassed 36-180 mg of curcumin. The outcomes of that examination proposed that curcuma extracts, even at the dose of 2200 mg is safe in a 4-month survey [91]. The other investigation used curcuminiod capsules at doses of 0.45-3.6 g/day for four months. Accordingly, no significant toxicity was observed cept for minor gastrointestinal effects in three of 15 patients [92]. A recent study has evaluated the effects of curcumin (500 mg) alone and in combination with diclofenac (50 mg) in 45 rheumatoid arthritis patients. It was proposed that curcumin at the used concentration has no adverse effect and thus is considered a safe supplementary therapeutic agent [93]. Lao and colleagues have examined the impact of escalated doses of curcumin in 24 healthy subjects. In this study, the escalating doses of curcumin (500-1200 mg) were administrated, and the safety of the drug was monitored for the next 72 h. The results showed that diarrhea and headache were seen in 30% of the individuals, not in connection with dose [94].
Then, based on the studies, the daily utilization dosage of curcumin appears to be safe up to 8 g per day for 3 months, excluding some persons that showed slight gastrointestinal side effects in one study. Besides, there is no report showing momentous toxicity for healthy subjects using 1.2 g of curcumin from the oral route for 3 days.
Probable clinical side effects of curcumin
Curcumin does not appear to have any side effects once used at a high dose of eight grams, but there are a few things to keep in mind while using curcumin in clinical use. When applied to mouse oocytes, curcumin was shown to block the meiotic restart of the oocyte and the process of mitotic cleavage by altering the spindle structure in a dose-dependent wayit did not cause any damage to the DNA. When combined with cytochrome P450 [95], curcumin caused DNA fragmentation. This means that further research is needed to determine curcumin's clinical safety before being used on a large scale. Chen and colleagues observed that curcumin reduced CYP1A2 by 28.6% and increased CYP2A6 by 41.8% in 16 healthy Chinese males. Curcumin lowered the plasma AUC of 1,7-dimethylxanthine (17X) by 27.2 percent, showing that it might alter 17X's pharmacokinetic characteristics. Hence, in clinical practice, the interaction between curcumin and other medications should be considered.
New techniques to improve curcumin's bioavailability
Curcumin has a low bioavailability, as previously stated, attributable to its low absorption and fast metabolism. Curcumin's low bioavailability would significantly reduce its bioactivity, thus limiting its therapeutic usefulness. Enhancing bioavailability is the primary issue that must be addressed in the use of curcumin [96,97]. Preclinical trials indicate that the bioavailability of curcumin may be increased by combining it with an adjuvant [98,99] or by using various drug delivery approaches. Additionally, an increasing number of experts have lately focused on curcumin's structural alteration to address the issue of bioavailability. These techniques, however, are seldom explained in person. The following text will outline different investigated ways to increase curcumin's bioactivity.
Integrating curcumin in nanocarriers via different methods is a suitable and constructive choice to increase its biological actions that improve its bioavailability and solubility, long-term circulation, preservation in the body, and overcoming its physiological limitations. In addition, it may decrease undesirable toxicity to neighbor healthy cells/tissues [100].
Liposomes are one of the best delivery carriers due to their ability to entrap an extensive diversity of hydrophilic and hydrophobic agents [27]. In a research work, liposomes enhanced the oral bioavailability of curcumin with higher Cmax and shorter Tmax. Furthermore, there was an increase in the oxidant activity in the plasma [101]. Another study proved the higher therapeutic efficacy of curcumin liposomes against human pancreatic carcinoma cells compared with plain curcumin [102]. Curcumin liposomes were reported to downregulate the activation of NF-κB, suppress cancer cell growth, and induce apoptosis in human pancreatic carcinoma cells in vitro [103]. More importantly, curcumin liposomes inhibited pancreatic carcinoma progression and suppressed tumor angiogenesis in vivo murine xenograft models [104]. The beneficial effectiveness of curcumin liposomes have been examined in many other cancers. Li et al [105] established that curcumin liposomes can prevent the growth of colorectal cancer cells compared with oxaliplatin, a chemotherapeutic agent used to treat colorectal cancer. Curcumin liposomal formulation exhibited a dose-dependent inhibitory effect on head and neck squamous cell carcinoma [106]. Many studies conducted on curcumin liposomes have been reported for their bioactivity on cancers. However, there have been rare reports of the safety of this type of curcumin. Numerous reports have also shown the results of curcumin-phospholipid complex as a carriage system to advance the therapeutic efficacy of curcumin. This complex increased the bio-absorption of curcumin, enhanced the curcumin's plasma levels in rats [27, 107] and protected the rat's liver fromoxidant damage [107].
Conclusion
For thousands of years, people have been using curcumin, which is a naturally occurring polyphenol. Curcumin has been found to have a number of activities both in vivo and in vitro, including cell proliferation inhibition, antioxidant activity, anti-cell adhesion, anti-angiogenesis, and antibacterial characteristics. It has been shown in previous clinical trials that curcumin is an effective anti-inflammatory and anti-tomur agent. Curcumin, on the other hand, has poor systemic bioavailability. Other conditions, such as neurodegenerative disease, cardiovascular disease, and diabetes, should be the subject of additional clinical research in the future. Furthermore, many techniques, such as adjuvants, drug delivery systems, and structural changes, should be used on people.
Acknowledgments
Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran, provided financial support for this research that is extensively acknowledged (grant number: 66511).
Orcid:
Solmaz Maleki Dizaj: https://orcid.org/0000-0003-4759-7222
Simin Sharifi: https://orcid.org/0000-0002-3020-3779
Shahriar Shahi: https://orcid.org/0000-0003-4616-5145
Soheila Montazersaheb:
https://orcid.org/0000-0001-5010-7293
Sara Salatin: https://orcid.org/0000-0001-9107-5603
Elham Ahmadian: https://orcid.org/0000-0002-7230-0489
Khadijeh Khezri: https://orcid.org/0000-0002-4671-985X
Yalda Rahbar Saadat: https://orcid.org/0000-0002-3295-404X
Elaheh Dalir Abdolahinia:
https://orcid.org/0000-0002-3168-7998
Mohammad Ali Ghavimi:
https://orcid.org/0000-0002-6638-2799
--------------------------------------------------------------------------
How to cite this article: Solmaz Maleki Dizaj, Simin Sharifi, Shahriar Shahi, Soheila Montazersaheb, Sara Salatin, Elham Ahmadian, Khadijeh Khezri, Yalda Rahbar Saadat, Elaheh Dalir Abdolahinia, Mohammad Ali Ghavimi*. The most important consideration in clinical usage of curcumin. Eurasian Chemical Communications, 2022, 4(2), 124-136. Link: http://www.echemcom.com/article_143047.html
--------------------------------------------------------------------------
Copyright © 2022 by SPC (Sami Publishing Company) + is an open access article distributed under the Creative Commons Attribution License(CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

.png)
